Putting the flow back in your workflow.
Say goodbye to duct-taped tools and disconnected systems. Drive engagement and enhance the attendee experience in one cohesive, easy-to-use platform.

Trusted by thousands of event planners worldwide.










































































































































Simple where it matters. Powerful where it counts.
Powerful tools that help planners breathe easier and give attendees a reason to smile.
Effortless for you.
Create, customize, and launch your event with ease. No bloated tech stack or repetitive manual tasks.

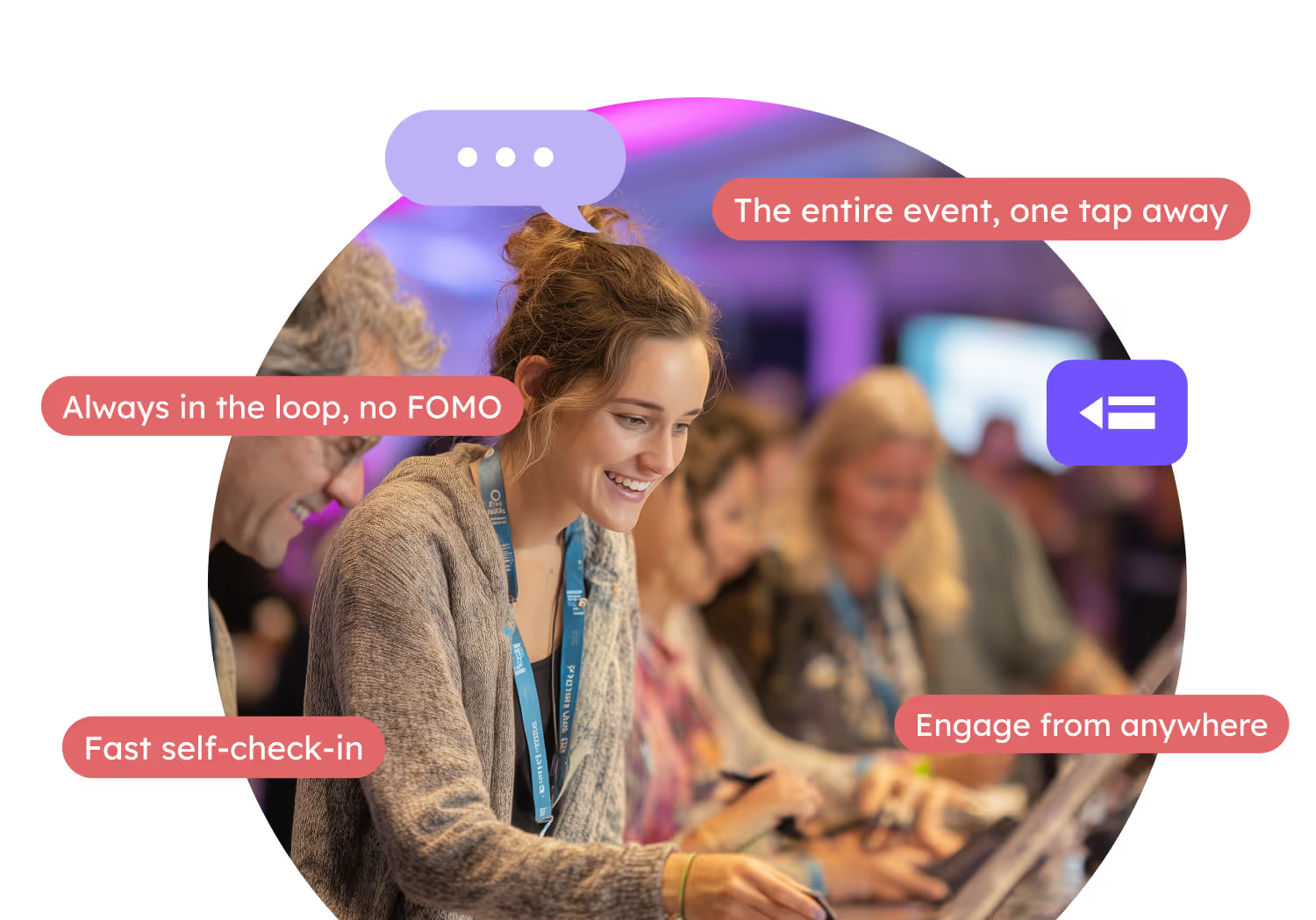
Delightful for them.
No scrambling or awkward “where am I supposed to be?” moments. Just a clear path from check-in to connection.
Built for the full event journey.
From pre-event buzz to post-event takeaways, Guidebook helps you deliver memorable event experiences from start to finish.
Promote
Create anticipation with an event website that’s on-brand and online in minutes.

Register
One streamlined system for tickets, payments, and gathering the right attendee data.

Engage
Keep attendees active and connected in your event app with live polls, gamification, push notifications, AI-powered networking, and more.

Track
Track attendance, engagement, and more with real-time dashboards that keep you in the know.

Optimize
Turn your data into smarter planning. Use insights to improve events and keep your audience coming back.

Tools that do the heavy lifting, so you don’t have to.
These aren’t just features. They’re time-savers, stress-reducers, and attendee-pleasers that will earn you a well-deserved standing ovation.
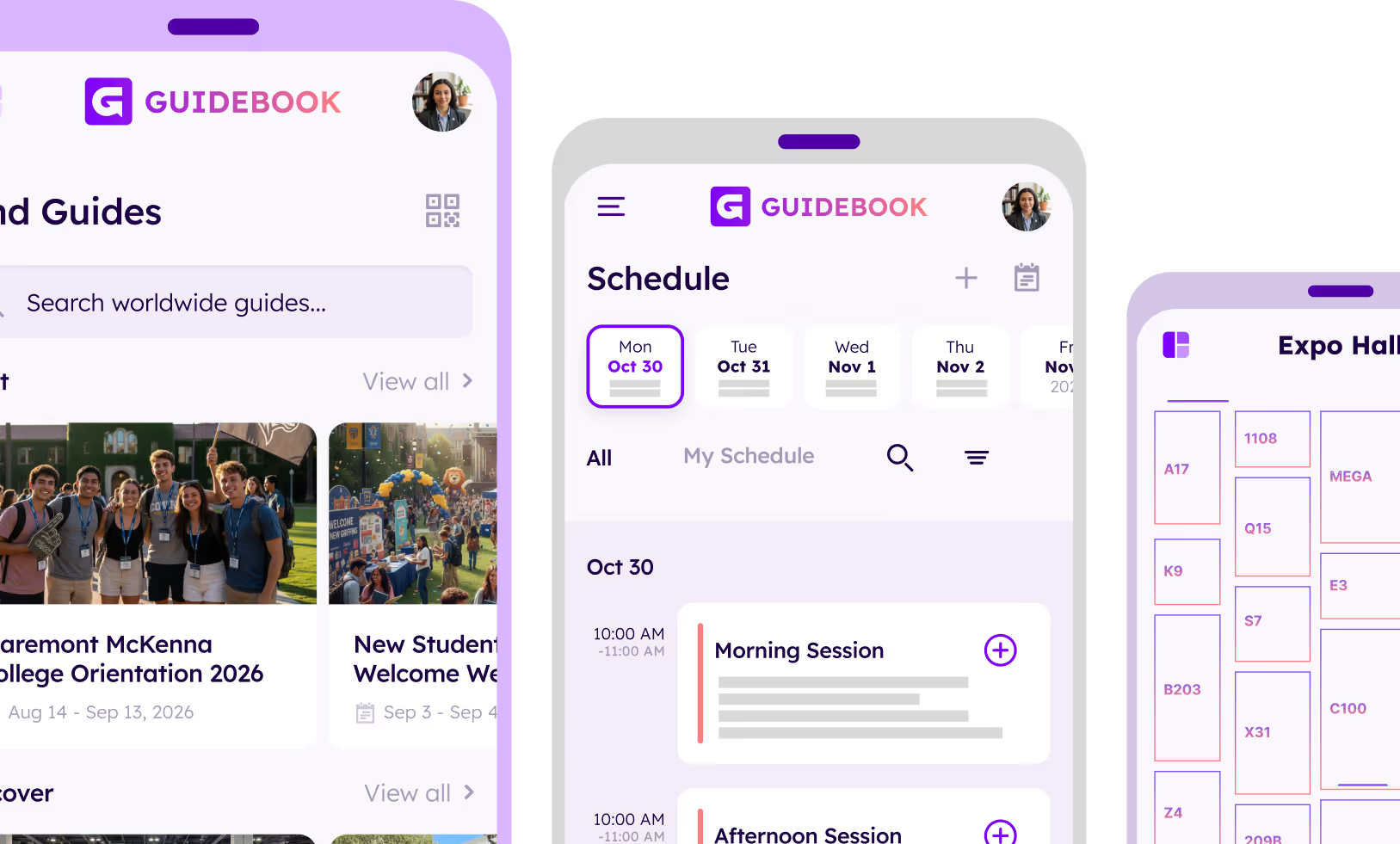
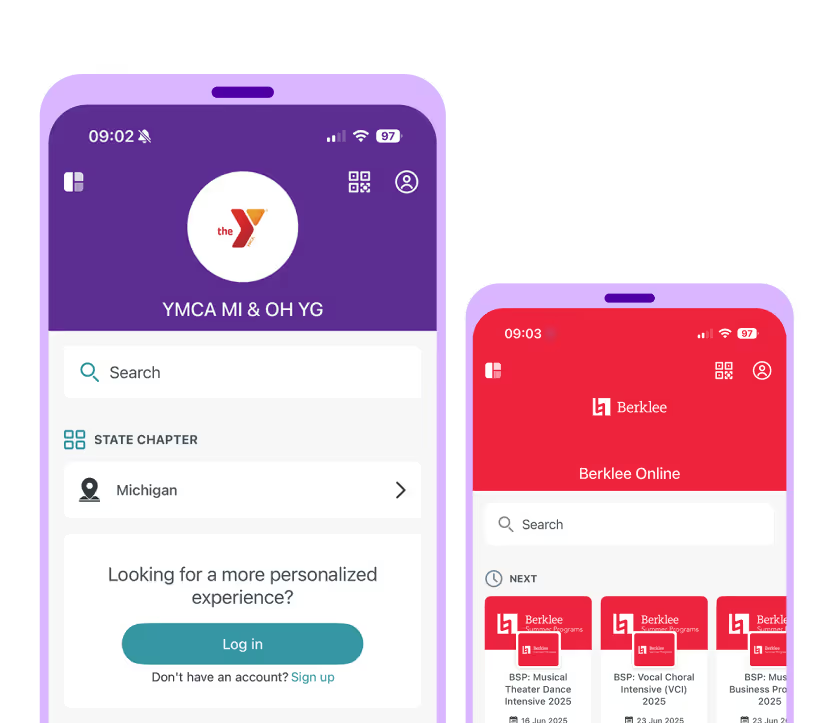
Build it yourself, no dev team required.
With an intuitive drag-and-drop builder, creating your event app is fast, visual (no coding), and entirely in your control.
Your brand, front and center.
Attendees see your logo, your colors, your voice — never ours.

Fits any event type.
From campus events to conferences to music festivals - if it brings people together, it belongs here.
Everything attendees need, just one tap away.
From personalized schedules to maps and messages, your attendees stay organized, connected, and confident throughout your event.
Works seamlessly with registration, websites, and badges.
Everything connects behind the scenes so you can save time and focus on delivering a great event.

Why choose Guidebook.
Powerful tools designed to make event management effortless.
Intuitive, stress-free workspace
Build your event app, registration, and more in a visual, drag-n-drop interface. No tech skills required.
All-inclusive pricing
You never have to worry about sneaky add-ons or paywalls. One price gives you access to everything you need.
Fully white-labeled experience
From registration to your event app, attendees see your brand only (never ours).
Works the way your team works
Manage access and build together without stepping on toes.

Your trusted partner for every event.
Proven across industries and event types, here’s what Guidebook has made possible.
Attendees connected through our platform
App downloads helping attendees engage and connect
Event planners building unforgettable experiences
Reviews celebrating our support and ease of use
Join 5000+ other
**event planners** today.
From Fortune 500s to universities to associations, teams trust Guidebook to save time, reduce chaos, and delight attendees.

See how it works




Trusted by top universities


Plan your next event with ease


Trusted by enterprises, associations and more